Summer 2017
The day I was diagnosed with Parkinson’s, in the summer of 2017, was one of the worst days of my life. Having left the doctors practice, I sat with my wife of six months, in a garden square in central London, and sobbed.
I was scared, my mind instantly painted a picture of “me” in the later stages of the disease, unable to care for myself, in a wheelchair, shaking uncontrollably. But I was most upset about the promises and plans I had made with my wife for the life we wanted to have together, and the things we wanted to do over the next 30 years or so, and feeling like I wouldn’t be able to make good on what we had agreed together on our wedding day in November 2016. I felt like I had let her down, and not only was my quality of life about to be thrown into turmoil, but hers too.
What I have since learned, is that whilst Parkinson’s is a progressive degenerative disease, the rate of progression may well mean that I have many able and active years to enjoy in the meantime. That is a curiously life affirming realization! Each day is precious, and we must (all of us) make the most of every day – before we are not able. So rather than fading away, I have grabbed every opportunity to make the most of life and do all the things that Jessie, and I want to do, personally and professionally.
Running with a dodgy shoulder
As a teenager I ran regularly, and came back to it in my early forties, culminating in running the London Marathon in 2013. And I still run today! My motivation was to stay fit and healthy and avoid some of the health pitfalls I had seen with my father and his heart. (I also have regularly done Pilates or Yoga and Spinning)
But shortly after the London Marathon I developed a pain in my left shoulder, which impacted my performance and made running far less enjoyable. After a few months of it not going away I went to see several shoulder specialists, who couldn’t quite seem to pinpoint precisely what was wrong.
They tried steroid injections a couple of times to ease the pain, but ultimately their belief was that surgery would be needed, after a couple of MRI scans. I underwent something called “subacromial decompression”, which is about shaving down the bone in your shoulder to create more space for your shoulder to move. This was followed by 6 months of physio, where I built up the muscles in my shoulder again. At the end of all that I tried to get back to running and whilst the pain was mildly improved, I still got a twitch in my shoulder at about 1.5 miles into any run I did. My shoulder joints would seem to get rigid and immobile, as a consequence get tired, and then my shoulder would start spasming arrhythmically. The exact same thing each time I ran at exactly the same place on my loop around Regents Park in London – just before the entrance to the Zoo!
My Physio and Shoulder specialist said they couldn’t understand it, and maybe this was being caused by damage in my neck. The neck specialist, decided to do an MRI guided injection of steroids in my neck, between C3 and C4 of my spine. That was really unpleasant! The view was this would fix my shoulder. But nothing changed, still the same issues remained.
Many doctors’ appointments and physio sessions later, we were all at a loss to understand what was going on. My Physio suggested that maybe the problem was neurological, as sometimes when a joint is in trauma for long periods of time, the brain starts to send different messages, than those normally sent, to the muscle group – in an attempt to protect that part of your body. His suggestion was that a neurologist might be able to identify this and use Botox to “turn off” the muscles to give the brain the chance to reset. It seemed like a long shot, but by now I was desperate to get fixed and resume running longer distances again.
Diagnosis
So, after four years of searching for a resolution, in the summer of 2017, I ended up at the offices of a prominent London based neurologist, with a specialism in movement disorders. In his mind I think he knew immediately what my problem was, he made me walk down his hallway, and saw that by now my left arm really wasn’t swinging like my right arm. He said my problem could be caused by several things, including brain tumor, or the result of an impact to my head, or Parkinson’s. To be sure he asked me to get an MRI scan and DAT scan completed, the later would show if I had Parkinson’s or not. I had blissfully entered his office thinking he was going to give me a shot of Botox in my shoulder, and left with trepidation, with the possibility of something much more serious – a tumor or Parkinson’s disease. My world was turned upside down!
I was back at the specialist a month or so later, with my scan results, for him to interpret and make his diagnosis. At the start of the meeting he didn’t make any diagnosis at all, he just started talking about the lack of dopamine in my brain and what that meant to me. I stopped him and said, “so what you’re saying is I have Parkinson’s?”. He said yes that’s what I had, that it was very clear from the scan, but that these days with treatment, the outlook as not as bad as I may be led to believe.
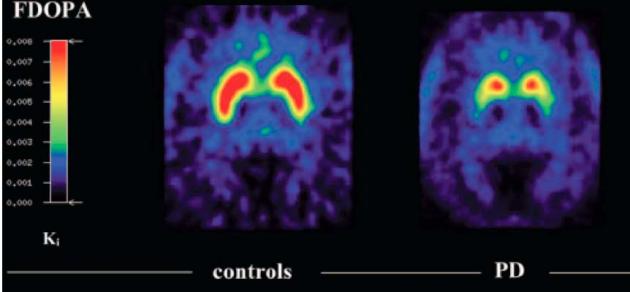
I asked if it was possible, he had it wrong and whether I should consider a second opinion? He spun the screen around that he was using to look at my DAT scan results, which showed the dopamine producing area of my brain, which should have been “peanut” shaped in each hemisphere, but were more circular; as parts were slowly dying off, reducing the production of dopamine in my brain (dopamine is essential for our brains to transmit the signals our bodies need, amongst other things, to move!). Basically, he was saying, you can get a second opinion, but this is so clearly Parkinson’s there is little point!
As we left the surgery, I could hardly walk straight, my mind was spinning, and all I could visualize was what I had read on the web, from google searches, and that was a much darker image than the doctor had just painted. I thought maybe he was just trying to soften the blow. Jessie and I walked across the road into the sunny garden square, and we sat there for a long time crying and holding each other.
Two years have gone by, and so far, the doctor seems to have been right. I’m not special, but I am not prepared to be defined by my disease. I continue to run a software company, exercise, travel and spend time with my family. With decent medicine, good routine, enough sleep, exercise and a good diet, I have mostly been incredibly well and VERY active.
Of course, being invited to move to the Netherlands to be a CEO of a Software company introduced more than a little extra complexity. Especially happening right at the same time. Initially, because of my own bias and “prejudice”, I was concerned as to whether I would be well enough to do a stressful job, but as the months rolled by my confidence rose as I gained better knowledge of what I was dealing with. So if you have had a recent diagnosis, and this story seems familiar to you, there is hope and you can continue to live a rich and full life, don’t let Parkinson’s define you. #stirrednotshaking





No Comments